Current Methods of Brain Electrode Placement
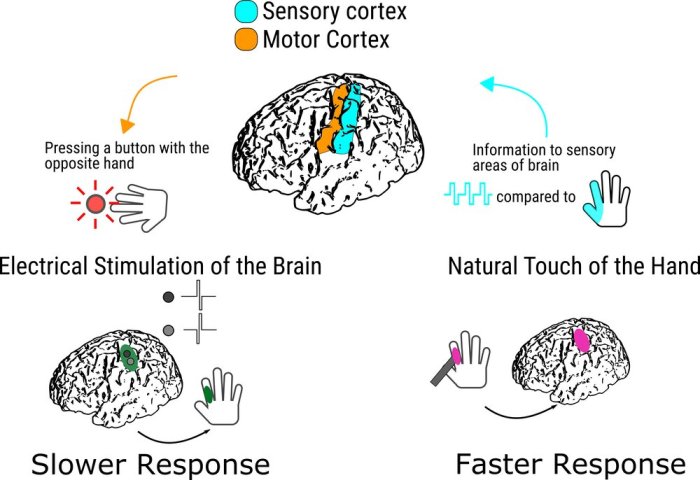
Brain-computer interfaces (BCIs) are a rapidly developing field with the potential to revolutionize how we interact with the world. These devices allow individuals to control external devices, such as computers or prosthetic limbs, using only their thoughts. A crucial component of BCIs is the placement of brain electrodes, which allow for the recording and stimulation of neural activity. While advancements in technology have led to less invasive methods, the current methods for placing brain electrodes still pose risks and limitations.
Stereotactic Electroencephalography (SEEG)
Stereotactic electroencephalography (SEEG) is a minimally invasive technique used to record brain activity directly from deep brain structures. SEEG involves surgically implanting electrodes into the brain through small holes drilled in the skull. These electrodes are then connected to a recording device outside the body.
SEEG is often used to diagnose and treat epilepsy, as it allows for precise localization of seizure activity. It is also used in research to study brain function and investigate the neural basis of various cognitive processes.
Advantages of SEEG
- High spatial resolution: SEEG electrodes can be placed directly in the brain, allowing for recordings of neural activity with high spatial resolution. This provides a more detailed picture of brain activity compared to other methods, such as electroencephalography (EEG).
- Long-term monitoring: SEEG electrodes can be left in place for extended periods, allowing for continuous monitoring of brain activity. This is particularly useful for studying epilepsy, as it allows for the identification of seizure patterns over time.
Disadvantages of SEEG
- Surgical procedure: SEEG requires a surgical procedure, which carries risks such as bleeding, infection, and damage to brain tissue.
- Limited reach: While SEEG provides high spatial resolution, the number of electrodes that can be implanted is limited. This may restrict the ability to record activity from all relevant brain areas.
- Cost: SEEG is a complex and expensive procedure, which may limit its accessibility to all patients.
Electrocorticography (ECoG)
Electrocorticography (ECoG) is a technique that involves placing electrodes directly on the surface of the brain. This method is typically used in patients undergoing brain surgery, as it allows for the mapping of brain function before surgery.
ECoG is often used to treat epilepsy, as it allows for the identification of seizure foci. It is also used in research to study brain function and investigate the neural basis of various cognitive processes.
Advantages of ECoG
- High spatial resolution: ECoG electrodes are placed directly on the brain surface, providing high spatial resolution recordings of neural activity. This allows for a more detailed picture of brain activity compared to other methods, such as EEG.
- Long-term monitoring: ECoG electrodes can be left in place for extended periods, allowing for continuous monitoring of brain activity. This is particularly useful for studying epilepsy, as it allows for the identification of seizure patterns over time.
Disadvantages of ECoG
- Surgical procedure: ECoG requires a surgical procedure, which carries risks such as bleeding, infection, and damage to brain tissue.
- Limited reach: ECoG electrodes are placed on the surface of the brain, which limits the ability to record activity from deep brain structures.
- Cost: ECoG is a complex and expensive procedure, which may limit its accessibility to all patients.
Electroencephalography (EEG)
Electroencephalography (EEG) is a non-invasive technique that involves placing electrodes on the scalp to record brain activity. EEG is a widely used tool for diagnosing and monitoring various neurological conditions, including epilepsy, sleep disorders, and brain tumors.
Advantages of EEG
- Non-invasive: EEG does not require surgery, making it a relatively safe and convenient method for recording brain activity.
- Widely available: EEG is a widely available and relatively inexpensive technique, making it accessible to a large population.
- Portable: EEG equipment is portable, allowing for recordings to be taken in various settings, such as hospitals, clinics, and even at home.
Disadvantages of EEG
- Low spatial resolution: EEG electrodes are placed on the scalp, which limits the ability to record activity from specific brain regions. The signals recorded by EEG are a composite of activity from multiple brain areas, making it difficult to pinpoint the exact source of the activity.
- Susceptible to artifacts: EEG recordings can be affected by artifacts, such as muscle activity, eye movements, and electrical interference. These artifacts can make it difficult to interpret the EEG signals.
Magnetoencephalography (MEG)
Magnetoencephalography (MEG) is a non-invasive technique that measures the magnetic fields produced by electrical activity in the brain. MEG is a powerful tool for studying brain function, as it provides high temporal resolution and good spatial resolution.
Advantages of MEG
- Non-invasive: MEG does not require surgery, making it a relatively safe and convenient method for recording brain activity.
- High temporal resolution: MEG can record brain activity with high temporal resolution, allowing for the study of rapid brain processes.
- Good spatial resolution: MEG provides better spatial resolution than EEG, allowing for the identification of activity from specific brain regions.
Disadvantages of MEG
- Expensive: MEG is a very expensive technique, limiting its availability to research settings.
- Susceptible to artifacts: MEG recordings can be affected by artifacts, such as electrical interference and magnetic fields from the environment.
Functional Magnetic Resonance Imaging (fMRI)
Functional magnetic resonance imaging (fMRI) is a neuroimaging technique that measures brain activity by detecting changes in blood flow. fMRI is a powerful tool for studying brain function, as it provides high spatial resolution and good temporal resolution.
Advantages of fMRI
- Non-invasive: fMRI does not require surgery, making it a relatively safe and convenient method for studying brain activity.
- High spatial resolution: fMRI provides high spatial resolution, allowing for the identification of activity from specific brain regions.
- Good temporal resolution: fMRI can record brain activity with good temporal resolution, allowing for the study of brain processes over time.
Disadvantages of fMRI
- Expensive: fMRI is a very expensive technique, limiting its availability to research settings.
- Limited temporal resolution: While fMRI provides good temporal resolution, it is not as fast as MEG or EEG. This makes it less suitable for studying rapid brain processes.
- Susceptible to artifacts: fMRI recordings can be affected by artifacts, such as movement and physiological noise.
Factors Contributing to Electrode Damage
Brain electrode placement, a critical step in various neurological procedures, can unfortunately lead to tissue damage if not performed meticulously. This damage can arise from various factors, including the electrode material, insertion technique, and the inherent fragility of the brain tissue itself. Understanding these factors is crucial for minimizing damage and ensuring successful outcomes.
Electrode Material and Design
The material and design of the electrode significantly influence the extent of tissue damage.
- Material Properties: The material’s biocompatibility, stiffness, and surface properties play a crucial role. For example, electrodes made of rigid materials like stainless steel can cause more trauma during insertion compared to flexible materials like platinum or iridium.
- Electrode Design: Sharp edges, protruding points, and rough surfaces can exacerbate tissue damage. Microelectrodes with smaller diameters and smoother surfaces are generally preferred for minimizing trauma.
Insertion Technique
The technique used to insert the electrode is another key factor.
- Insertion Angle and Depth: Inserting the electrode at an incorrect angle or exceeding the intended depth can lead to damage to surrounding structures.
- Insertion Speed: Rapid insertion can cause significant trauma to delicate brain tissue. Slower, more controlled insertion techniques are generally recommended.
- Surgical Precision: Minimizing the number of insertions and ensuring precise placement are essential to minimize the overall damage.
Brain Tissue Properties, Brain electrodes less damaging placement
The brain’s delicate nature and susceptibility to injury must be considered.
- Tissue Fragility: Brain tissue is highly fragile and prone to tearing or shearing during electrode insertion.
- Blood Vessel Density: The brain’s dense network of blood vessels can be easily damaged during electrode insertion, potentially leading to bleeding and inflammation.
Consequences of Electrode-Induced Damage
Electrode-induced damage can have a range of consequences, impacting the success of the procedure and the patient’s well-being.
- Neurological Deficits: Damage to brain tissue can lead to neurological deficits, such as impaired motor function, sensory loss, or cognitive impairment.
- Inflammation and Scarring: The insertion process can trigger an inflammatory response, leading to scar tissue formation that can hinder the long-term function of the electrode.
- Infection: Electrode insertion creates a pathway for infection, potentially leading to serious complications.
- Electrode Failure: Damage to surrounding tissue can affect the stability and function of the electrode, leading to premature failure.
Emerging Technologies for Less Damaging Placement
The quest for minimally invasive brain electrode placement has spurred the development of innovative technologies that aim to minimize damage to delicate brain tissue. These emerging approaches offer promising alternatives to traditional methods, paving the way for safer and more effective brain-computer interfaces (BCIs).
Minimally Invasive Electrode Placement Techniques
These techniques focus on reducing the invasiveness of electrode implantation by employing smaller and more flexible materials, as well as advanced delivery methods.
- Flexible Microelectrodes: These electrodes are made from materials like polymers or silicon, allowing them to conform to the shape of brain tissue. Their flexibility reduces the risk of tearing or damaging delicate neurons.
- Microfluidic Electrode Arrays: Microfluidic channels integrated into electrode arrays enable the delivery of drugs or other substances directly to the targeted brain region. This approach can reduce inflammation and improve electrode stability.
- Biocompatible Materials: Advancements in biocompatible materials, such as conductive polymers and bioresorbable materials, enhance electrode integration with brain tissue, reducing the risk of rejection and long-term complications.
Electrode Placement Guided by Imaging Techniques
Leveraging advanced imaging technologies to visualize brain structures in real-time enhances the precision of electrode placement.
- Intraoperative Magnetic Resonance Imaging (iMRI): iMRI allows surgeons to monitor brain tissue in real-time during surgery, enabling precise electrode placement and minimizing the risk of damaging critical areas.
- Electroencephalography (EEG)-Guided Navigation: EEG signals can be used to guide electrode placement, ensuring that the electrodes are positioned in regions with optimal electrical activity.
Robotic-Assisted Electrode Placement
Robotics can enhance the accuracy and precision of electrode placement, reducing human error and minimizing tissue damage.
- Robotic Surgical Systems: Robotic systems equipped with advanced imaging and navigation capabilities allow surgeons to precisely place electrodes with minimal tissue manipulation.
- Microrobots for Electrode Delivery: Microrobots, guided by magnetic fields or other external stimuli, can deliver electrodes to specific brain regions with high precision, reducing the need for large surgical incisions.
Research and Development in Minimally Invasive Techniques
The pursuit of less invasive brain electrode placement techniques is driving significant research and development efforts, aiming to minimize the risks and improve the long-term efficacy of neurotechnology. These advancements hold the promise of safer and more effective treatments for a wide range of neurological conditions.
Minimally Invasive Techniques for Electrode Placement
Minimally invasive techniques are designed to reduce tissue damage and improve patient outcomes. They involve smaller incisions, targeted delivery, and advanced imaging guidance, allowing for more precise electrode placement.
Stereotactic navigation systems use advanced imaging techniques, such as CT scans and MRI, to create a 3D map of the brain, enabling precise electrode placement. Robotic guidance systems further enhance accuracy by automating the insertion process, minimizing human error.
These technologies offer greater precision and control, reducing the risk of damaging critical brain structures.
2. Microelectrode Arrays
Microelectrode arrays are small, flexible devices containing multiple electrodes that can be implanted in specific brain regions. Their small size and flexibility minimize tissue disruption and improve electrode integration with the brain.
Microelectrode arrays are particularly useful for recording neural activity from small, localized brain regions.
3. Biocompatible Materials and Coatings
Researchers are developing biocompatible materials and coatings for electrodes to enhance their integration with brain tissue. These materials aim to minimize inflammation, promote tissue regeneration, and improve the long-term stability of electrodes.
Biocompatible materials and coatings can reduce the risk of electrode rejection and improve the long-term performance of implanted devices.
4. Wireless and Implantable Devices
Wireless and implantable devices are being developed to eliminate the need for external wires and connectors, further reducing the risk of infection and tissue damage. These devices allow for long-term monitoring and stimulation of brain activity without the need for surgery.
Wireless and implantable devices offer greater convenience and improved patient comfort, enhancing the practicality of neurotechnology.
Challenges and Potential Solutions
While minimally invasive techniques offer significant advantages, there are still challenges to overcome.
1. Accuracy and Precision
Achieving precise electrode placement remains a challenge, especially in complex brain regions. Advanced imaging techniques, robotic guidance, and intraoperative imaging can further enhance accuracy.
2. Biocompatibility and Integration
Long-term biocompatibility and integration of electrodes with brain tissue are crucial for maintaining device function and preventing complications. Continued research on biocompatible materials, coatings, and device design is essential.
3. Durability and Reliability
The durability and reliability of implanted electrodes are critical for long-term applications. Advanced materials, robust manufacturing processes, and improved device design are key to ensuring long-term functionality.
4. Minimizing Surgical Risks
Minimally invasive techniques aim to reduce surgical risks, but complications can still arise. Continued research and development of safer surgical procedures, improved patient selection, and careful post-operative monitoring are crucial.
Future Directions and Potential Applications: Brain Electrodes Less Damaging Placement
The development of less damaging brain electrode placement techniques opens a vast array of possibilities across diverse fields, revolutionizing our understanding of the brain and its potential. These advancements pave the way for groundbreaking medical treatments, enhance the scope of neuroscience research, and unlock the potential of neurotechnology.
Medical Treatments
Less invasive electrode placement holds immense promise for improving the lives of individuals with neurological conditions. These techniques could lead to more effective and personalized treatments for a wide range of disorders, including epilepsy, Parkinson’s disease, and Alzheimer’s disease.
- Epilepsy: Precisely targeted electrodes could provide more accurate monitoring and stimulation of brain regions associated with seizures, enabling more effective seizure control and reducing the need for invasive surgery.
- Parkinson’s disease: Deep brain stimulation (DBS) using less invasive electrode placement could offer a more targeted and efficient treatment for tremors, rigidity, and other motor symptoms, improving quality of life for patients.
- Alzheimer’s disease: Electrodes strategically placed in brain regions involved in memory and cognition could potentially help monitor disease progression and explore new therapeutic strategies to slow or reverse cognitive decline.
Neuroscience Research
Less damaging electrode placement techniques empower neuroscientists to delve deeper into the complexities of the brain, fostering groundbreaking discoveries and advancing our understanding of brain function.
- Neural activity mapping: More precise and minimally invasive electrode placement allows for detailed mapping of neural activity across different brain regions, revealing intricate patterns and connections that were previously inaccessible.
- Brain-machine interfaces: Less invasive electrode placement could facilitate the development of more sophisticated brain-machine interfaces (BMIs), enabling direct communication between the brain and external devices. This could revolutionize the treatment of paralysis, blindness, and other neurological impairments.
- Cognitive neuroscience: By allowing for longer-term and less disruptive monitoring of brain activity, less invasive electrode placement opens up new avenues for investigating complex cognitive processes, such as memory, attention, and decision-making.
Neurotechnology
The development of less invasive electrode placement techniques is poised to accelerate the advancement of neurotechnology, leading to a future where humans can interact with technology in unprecedented ways.
- Brain-computer interfaces (BCIs): Less invasive electrode placement could enable the development of more intuitive and user-friendly BCIs, allowing individuals to control devices and interact with the digital world using their thoughts. This could revolutionize communication, entertainment, and even healthcare.
- Augmented reality (AR) and virtual reality (VR): Less invasive electrodes could enhance the immersive experience of AR and VR by providing more natural and intuitive control over virtual environments. This could have profound implications for gaming, education, and training.
- Artificial intelligence (AI): Data collected from less invasive electrodes could provide valuable insights into brain function, aiding in the development of more sophisticated AI algorithms that mimic human cognitive abilities.
Brain electrodes less damaging placement – The quest for less damaging brain electrode placement is a testament to the power of innovation and the unwavering dedication of scientists and researchers. As we continue to push the boundaries of what’s possible, we can expect to see even more breakthroughs in this field. This is not just about developing new technologies; it’s about improving lives, enhancing our understanding of the brain, and paving the way for a future where brain disorders are no longer a barrier to living a full and meaningful life. The journey towards less damaging brain electrode placement is just beginning, and the future is bright.
Imagine the possibilities if brain electrodes could be placed with less damage, unlocking new frontiers in neurotechnology. It’s like the design revolution happening with smartphones – check out this oppo handset leaked with very thin bezel , where the bezels are practically nonexistent! Similarly, less invasive electrode placement could pave the way for more effective brain-computer interfaces, potentially revolutionizing how we interact with technology and even our own bodies.
 Standi Techno News
Standi Techno News